“Wellbeing with Welfare Technology”: Shuvarthi Bhattacharjee shares his reflections on his secondment at the Swedish tech start-up Posifon-AB
In early Spring 2023, I completed my secondment at Posifon-AB in Sweden. Posifon AB is a Swedish market leader in GPS alarms. The company creates new welfare services for citizens through mobile applications with GPS support that can be passively embedded into objects like bracelets, watch or sole in the shoe. Posifon AB is one of the secondment partners of the INNOVATEDIGNITY project with the aim to extend a practical experience to an Early-Stage Researcher (ESR) working in the domain of older people’s care and digital health technologies. Presently, Posifon AB has expanded to Norway and planning expansion plans in other countries. It is actively involved in creating cooperation with other technological enterprises across Sweden to strengthen its product portfolio.

An introductory e-mail from Posifon-AB read “Welcome to snowy Göteborg, Shuvarthi!!” and as I glanced through the train window, I could see a scenic snow capped landscape awaiting me. My secondment started on the following day with a warm welcome from the CEO of Posifon-AB, Mr. Henrik Essunger. The company offers a variety of GPS units, to wear as a bracelet, as a necklace or as a GPS SmartSole, a sole to put in the shoe (Please see Picture of the GPS units).

Mr. Niklas Granung, the Chief Operating Officer of Posifon-AB, detailed on the technology behind the functioning of the devices. Geofencing, he explains, is key to the functioning of the GPS-based alarms. It is a virtual geographical boundary that sends a trigger to the Posifon-AB care portal when a beneficiary (or user) exits a demarcated boundary. Once triggered, the older person is contacted by phone or in-person reached by a local social care worker requesting the person to return to safety. Ms Anna-Lena Frandeborn, who works in Posifon-AB, explained to me how she communicates frequently with a team of social care workers in various localities and she serves as a link liaisoning between the municipality and Posifon-AB. The process of identifying a particular product for a user is through a chart guided by persona based approach and the functionality desired by the client.
My next stop was at the Goteborg Municipality to meet Ms Asa Wall, the Planning Leader for Welfare Technology and attractive home care in the municipality. We discussed in detail the process for selection of vendors for welfare technologies like GPS-based alarms, the process of supporting such a city-wide technology-based intervention through call centres and future plans to include passive fall prevention sensors for older people at home.
Multiple perspectives garnered from the stakeholders offered me a comprehensive understanding of the entire process of operation. Retrospectively, I feel the key to Posifon-AB’s success lies with continuous technological upgradation, innovative solutions and above all, consensus-based team decisions. A lot of those innovative ideas actually came from informal meetings (Fika, A Swedish tradition to meet over cake and beverages in the afternoon).


During this secondment, I investigated the wearable devices industry in the UK, the process of delivering the products to the end users and the challenges faced at various levels (e.g. local council, healthcare providers, technological industry and care homes) in delivering such services to older people. Transferability issues are complex. Posifon-AB’s Swedish business model offered a template to contrast with the market leaders in the UK. The regular support received from Posifon-AB was phenomenal and this secondment helped me in garnering an actual field exposure exploring the wearable devices sector for older people first hand.
Abraham Kebede worked with the Digital Lab at KareInn, UK,and reflects on his secondment experience
As part of the work with INNOVATEDIGNITY, industrial placements have been given special emphasis as a way of learning and dealing with the practical aspects of the discipline one is researching. My research, which focuses on the older adults’ experience of dignity in relation to everyday and care technology, was an ideal fit for a placement in a care technology company that provides a digital care planning platform for residential and nursing homes.
During my twelve-week secondment, I had the opportunity to work with the service and implementation operation team and observe how they provide continuous support and coaching for the carers and care managers to enhance their skills and capabilities. I attended a practical training session aimed at the wider care team, where practical training sessions were conducted. From a theoretical perspective, I understand the importance of continuous support and coaching, rather than relying on a one-time installation, in achieving success, adoption, and scalability of care technology. Recognizing that carers may have varying levels of digital literacy and adaptability, it is crucial to establish a responsive system for collecting feedback and addressing issues as they arise while offering continuous education and digital support.
I also participated in a digital adoption club, a unique series of events where developers, the operating team, and customers come together to explore ways of improving the product experience, provide feedback on necessary modifications, and assess its performance.
I had the opportunity to engage in a conversation with the Chief Product Officer, who has extensive experience in software development. He reflects what makes a technology designed for care and humans successful, adopted, accessible, and enjoyable for both intermediate and end users. He emphasized the importance of developing an intuitive product and minimizing cognitive load as a possible intervention to make complex systems simple and reduce the burden of carers.
During my secondment with KareInn, I authored two blog posts for KareInn’s social media relating to my experiences with the service implementation department and the development and product side of the business.
I would like to extend special thanks to Rachel Stovenic for supervising and organizing an excellent plan for me to gain experience from every aspect of the organization and the product. I would also like to express my gratitude to the Chief Product Officer, Phil, for his time and insights. Finally, I appreciate the support of Rachelle Mills, CEO of KareInn, for facilitating this secondment.
Please watch a short video of me speaking with Chief Product Officer Mr. Phil Brown. In this video vlog we discussed about his experience and background in software development, the uniqueness and value propositions of KareInn and care technologies in general.
“Listening to relatives” – Jessica Enros’ secondment at a National Competence Centre for Relatives (NKA) in Sweden
Some reflections about my secondment during INNOVATEDIGNITY EU-project from Linneaus University, Växjö in Sweden. NKA is a National competence centre for relatives – for a ‘relatives-friendly society’. The main assignment for NKA is to be an expert support to municipalities, county councils and individual providers regarding family support issues and to provide knowledge support directly to parents and relatives of people, preferably children and relatives of people, with a combination of several extensive functional impairments and extensive medical needs. The responsibility for advice and support for individuals in general rests with the municipalities and county councils. The assignment includes that NKA shall contribute to higher quality and productivity in the area of relatives by support the implementation of family support, development of methods and tools, knowledge transformation and knowledge exchange, be a link between research, practice and decision-makers and to be Sweden´s point of contact when it comes to international cooperation in the area.
In operations, NKA must paying particular attention to gender-related differences and consequences in relative support, paying particular attention to relative support in an intercultural perspective, in particular contribute to facilitating the prerequisite for combining the role of relative with participation in working life and good health, support and develop the role and responsibility of the healthcare system in terms of support for relatives and lastly in case of children as relatives especially contribute to such support that the relatives’ difficulties do not interfere with the child’s health, development and schooling.
NKA is a collaborative resource for developing future relative support and started in 2008. Their operating ideas is to create and develop meetings between different forms of knowledge and experience as:
- First-hand experience of family carers, users and their organisations
- Practical experience with staff in relative support and elderly care
- Organizational and policy experience of decision makers
- Scientific knowledge and methodological knowledge of researchers.
During the secondment I contacted different psychiatric wards for elderly people around regions in Sweden. The small survey that I, as a research assistant made, was about finding out if the relatives to elderly people with severe mental illness did get any support from their psychiatric ward and what kind of support if it existed. This was the main point and the results around in Sweden did differ much. In some psychiatric wards they had support for relatives and that could for example be a support group or individual meetings together with mainly a counsellor. As anticipated some of the support was sporadic underlining the need to find ways to listen to relatives and the importance of advocacy organisations such as AKA.
“No one should be alone with cancer.” – Mavis Bengtsson’s secondment at Kraftenshus in Sweden, exploring the process of co-design

Prof Andreas, Mavis (INNOVATEDIGNITY ESR) and Dr Erik at Kraftenshus, Boras, Sweden
As an Early-Stage Researcher (ESR) from INNOVATEDIGNITY Project, based at Bournemouth University, England, I undertook my secondment in Kraftenshus in Boras, Sweden and was under the mentorship of Professor Andreas Hellström and Dr Erik Eriksson. They have been instrumental in initiating Kraftenshus through research and evaluation that informed decisions in Kraftenshus. Kraftenshus is based in Boras, and it is the first support centre in Sweden designed by and for people affected by cancer, including patients, family, friends, staff members and local community representatives. My PhD is about older peoples’ perspectives about the design of care services, particularly care service as live in home, so it was interesting to experience another organisation with a similar goal and to learn about their experiences of co-design. My own study used a co-design process with older people and it was interesting to compare processes and learning from both initiatives and in a cross national context. A core principle in both areas of work in the UK and Sweden focused on homeliness and sense of home.
The founder of Kraftenshus experienced that after being diagnosed with cancer and getting her chemotherapy, she lacked support in the community, where she experienced loneliness. However, starting this organisation to help other cancer patients improved her well-being. The organisation started in 2017 in Boras, Sweden and has recently expanded to 2 more cities.
The impact of cancer on individuals is profound, and diagnosis means emotional turmoil for most people, as it affects all aspects of health(Mohlin et al. 2020). Cancer patients often desire emotional support after a cancer diagnosis (Ray et al. 2019). These people who want support might not always receive it, even though emotional support can come from a range of people in their social networks (Ray et al. 2019). The complexities of cancer increase once people are back in the community because it affects the whole family. Most patients feel lonely, and Kraftenshus helps patients to meet other patients. As the population ages, more people will need this crucial support.
The organisation’s core focus is on emotional and social support for people with cancer. The design of the venue was based on the action research results. It was valuable for me learn about the process Kraftenhus used and their particular methodological approach to co-design, that worked for them in practice and led to informing the shape of service delivery offered.
The meeting place is designed as a home to give people a homely feeling when they discuss their issues. The organisation and activities are a patient-led and voluntary organisation. They received funding from the government in 2017. Kraftenhus use a participation and co-creation model and a service design approach. They have considered a sustainable business model to establish how the project would survive over the years. One of the areas was creating a shared vision with the politicians and other stakeholders. With resources from the Universities, they have evaluated the organisation.
Members volunteer and lead activities or teachings. They collaborate with various stakeholders, do knitting, have creative painting rooms, do walks, have a gym membership, and get referrals from the hospital. Kraftenshus has a long collaboration with the Regional Cancer Centre, which drives the implementation of a cancer strategy launched in 2010 due to increased cancer cases and challenges of the healthcare system in Sweden. Kraftenhus worked closely with Regional Cancer Centre to design an integrated and patient-oriented cancer care model in the community.
One of the areas that we explored with Prof Andreas Hellström and Dr Erik Eriksson was to do further research at Kraftenshus together.
Kraftenshus is a valuable community organisation contributing to cancer patients’ emotional healing and with the motto: “No one should be alone with cancer.”
To find out more about the wonderful work Kraftenshus does visit their website.
Adam Nyende on his time with the Royal College of Nursing (RCN)
Adam Nyende carried out a secondment with the Royal College of Nursing (RCN) from September to November 2020 as part of the project. As this project provides training for 15 doctoral researchers to contribute to the next generation of leaders to deliver innovations in dignified sustainable care systems for older people, opportunities to work with professional organisations who engage in policy work was central.

Due to the Covid19 restrictions the training was held virtually with engagement with teams and various speakers each week from different academic and professional fields who discussed a range of academic and practice aspects such as work force policy, chellenges for older people and professional issues to support these challenges.
As well as the direct training the programme provided insights to the diverse work of the RCN, particularly its policy influence agenda and influential methods. In addition, the placement offered a unique opportunity to understand the inner workings of the Royal College of Nursing, including working with professionals in various departments on different aspects such as diversity and inclusion, policy-making, information and library, and public affairs . This was a great opportunity to enhance professional network and improved confidence working with non-academic professionals/partners.
Beyond sharing their expertise and perspectives on several relevant aspects, the professionals showed keen interest in Adam’s doctoral research work offering continued facilitation andproviding support the months ahead, particularly in a policy assignment concerned with workforce sustainability. Dr Dawne Garrett (RCN National Advisor for Older People at the time) ) was particularly hands on in offering guidance on designing the short policy focused project and signposting me to the available support and literature at the Royal College of Nursing (RCN).
The most critical new learning gained from the placement was the contextual understanding of how the nursing profession is structured and practised within the wider United Kingdom, particularly in England and how this impacts the design and delivery of older person care in the United Kingdom.
Adam learnt that nursing in England is a highly regulated profession with structures and systems to ensure quality and ethical care service delivery. Furthermore, unlike in some other parts of the world, there is a noticeable increase in the number of male nurses in England, and this could perhaps be attributed to the fact that the nursing profession continues to claim its position as one of the most critical components of the Health and Social Care Sector in England. Moreover, the nursing profession is still grappling with racial and gender inequalities, particularly regarding career progression opportunities. Finally, the nursing profession in England highly depends on the immigrant workforce, and this has triggered further debates on workforce retention and sustainability, particularly during the Covid-19 and post-Brexit era.
The key take-home message from the secondment, particularly the policy-making process, is that timing always affects policies. It is important to define what is important at a given time, in a current societal and national context. This is essential because no matter how good a policy might be, it will most likely not succeed if the timing is not right. Therefore, policy-making is about choosing the right issue(s), the right method(s), the right time, and the right target group(s). This will be an important message that Adam will take forward in his career in supporting dignified care for older people.
Panagiota Lafiatoglou reflects on her Secondment at the Physical Medicine and Rehabilitation Unit, University Hospital of Ioannina, Greece

In the winter of 2020 I undertook my three-month secondment in the Physical Medicine and Rehabilitation Unit (PMR) at the University Hospital of Ioannina, Greece. PMR Unit is the first University Rehabilitation Clinic in Greece and the first public medical department which operates as a rehabilitation center, offering specialised medical and rehabilitation services in Western and Northern Greece. The unique contribution of the PMR Unit lies on the provision of personalised rehabilitation programmes to patients which are tailored to the particular needs and health conditions of each individual.
During my secondment, I had the opportunity to immerse myself into the lived experiences of individuals diagnosed with brain injuries, witnessing in person their feelings, concerns and struggles during their inpatient rehabilitation. I also observed patients’ daily routines including their medical interventions and physical therapies.

Despite the difficulties caused by the COVID-19 pandemic and the lockdown restrictions at the time, the physiotherapy exercises for individuals were well-scheduled with no delays and disruptions. Another important aspect was the encounters I had with the patients’ relatives. The anguish and anxiety felt by relatives regarding the rehabilitation progress and recovery of their loved ones was overwhelming. I realised on the one hand how difficult this whole process is both for patients and their family members but at the same time how important family support can become during the inpatient rehabilitation of individuals living with brain injuries.
At the same time, I had the opportunity to build rapport with relevant stakeholders and consult with health professionals and experts on medical and nursing issues related to brain injuries. These fruitful conversations helped me immensely during my research, facilitating in particular the process of my fieldwork of my PhD thesis which aims to contribute to the strengthening of health service delivery in Greece. Overall, my secondment at the PMR unit was a constructive learning experience that allowed me to familiarise myself with the operation of hospital rehabilitation services in Greece, while also fostering my knowledge regarding my research topic.
What do nursing assistant students learn about well-being? Emma Jelstrup Balkin shares some thoughts…

“What do you think makes for a good quality of life for nursing home residents?” the teacher asks the class. It’s a cold and wet Tuesday morning in northern Denmark and I’ve just taken my seat in a classroom full of hopeful future carers – women of all ages, and one man. I’m here on secondment as part of my MSCA fellowship with InnovateDignity. SOSUNord is my secondment host. This is the college that trains nursing home care staff, among other things, and they have generously allowed me to observe some of their classes. This morning the class is supposed to be learning about welfare technologies, but the teacher, Jens is kindly taking some time out of their schedule to talk about well-being and dignity for nursing home residents. This is the topic that I am researching for my PhD, and it is fascinating to hear what these students – many of whom, in a year’s time, will be employed as nursing home staff – think about the well-being of those they will be caring for.
What I think was intended to be a ten-minute chat, turns into an hour-long discussion. Most of the students chime in. “Being seen and heard” says one. “Being respected by their carers” says another. They’re passionate and fresh from their first practical placement, they bring lots of newly gained experiences. Both good and bad. One student tells us that she spent a few hours making Christmas cookies with some residents and that doing this activity together gave them a chance to really talk. As their hands busily rolled the traditional Danish “pebernødder”, the memories of the past came rolling in thick and fast. She said it was so enjoyable being able to do this with them, and the regular staff appreciated it too as they never have the time for it themselves. Others told of less encouraging experiences, where the regular care staff were not interested in any new ideas. “Why don’t they do anything with residents in the evenings? They just put them all to bed at 8pm” one said with exasperation.
Though many of the students had had positive experiences, it is clear that there is still work to be done to ensure dignified care for all older people. Nonetheless, I was heartened to see that a new generation of care staff are approaching their work with such zeal for their charges. Care work is not easy. It demands a lot from the caregiver, physically, mentally and emotionally. It is underpaid and undervalued. But it is one of the most important responsibilities we have as a society: to care for one another.
In my research I attend to the lived experiences of the oldest old nursing home residents, in an attempt to grasp at what it is like to be really old and dependent on care in everyday life. I have learnt many things from my interlocutors, not least that it is not dependence that bothers them most. In fact, care dependency was a non-issue for most. What is important to them is mattering, being seen and heard as a person, a person in relation to other persons. While it is the oldest old’s own experiences that I center on in my research, it has been fascinating to learn about the other side of it during my secondment at SOSU Nord.
Rada Sandic Spaho’s Secondment experience
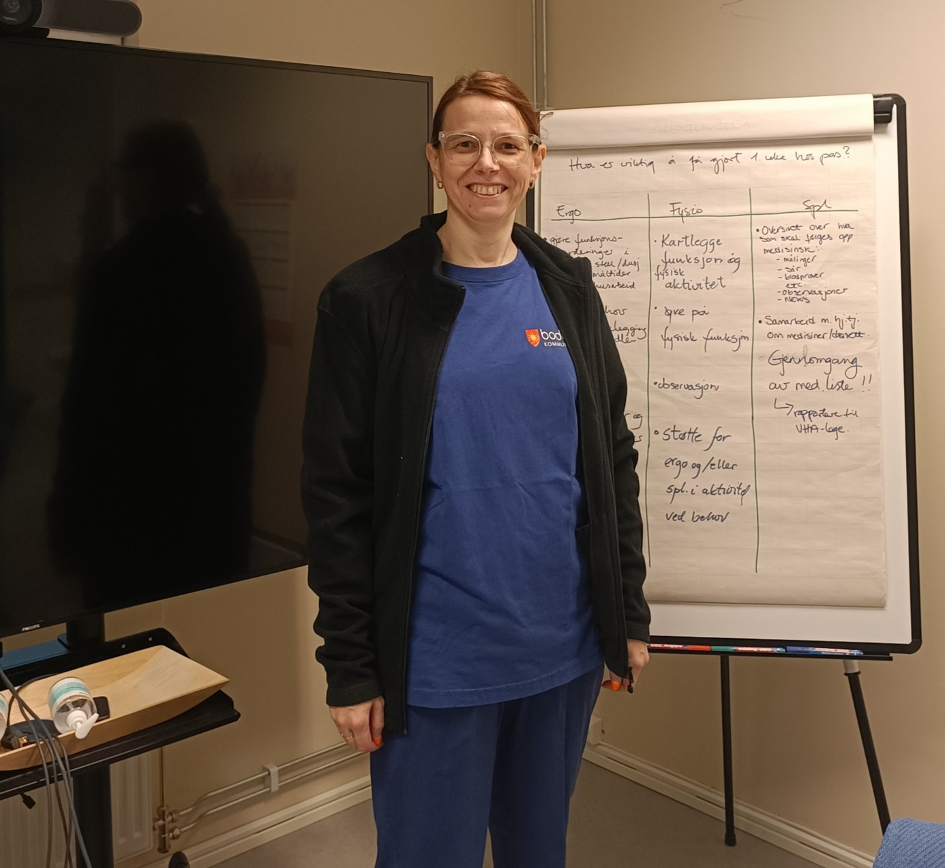
Rada Sandic Spaho had her 3 months secondment at the Virtual ward at Bodo municipality, Norway where she got to know more about this department and exchange knowledge with the team. The virtual ward is a multidisciplinary team consisting of a physician, an occupational therapist, a physiotherapist and 2 nurses. The project is led by a chief medical officer at the municipality. The team is organized in such a way that they perform home visits to patients following their discharge from the hospital. They assess and provide for the patient’s needs and care, and therefore prevent readmissions. What is amazing about this approach is that they get to assess the patients in the confines and safety of their own homes and environments, and the team are the guests. Each member of the team looks not only at the patient, but the house organisation, and family dynamics, and searches for ways to provide optimal care for the patient, such as ergonomic accessories, medications, exercises etc. In addition, the team is not very restricted by time constraints. They can talk to the patient for as long as deemed necessary in order to gain a holistic overview of the patient’s situation and build trust. This is to provide individualised, patient-centred care, which encompasses the patient’s social needs too. The team asks the patient if s/he likes to sing, walk, knit, play chess, etc. and provides information on organized gatherings that a patient can choose to participate in. The team provides a multidisciplinary assessment of the patient’s health condition and needs and can recommend or refer the patient to a higher level of care if need be.
Here is Rada’s experience: I learned how is it in practice to work with eHealth solutions, go through the messaging system, and how much time one needs to prepare (gather relevant information about the patient) before each visit, and patient interaction. It requires a lot of preparation, but also reflection following the visit. The team discusses and reflects on how each of them can contribute to the patient’s benefit and health improvement. I also got the insight that patients can have wearable devices but are often afraid to damage them. As an example, a safety alarm which consists of a single-button device that triggers a response from the monitoring unit. It is usually worn as a bracelet or necklace and should not be taken off. However, during a home visit to an elderly patient, we found that the patient was afraid to damage the device while showering and sleeping with it on. She, therefore, kept it in her drawer for safekeeping. She was very relieved when she was told that she cannot damage it and ought to always have it on her person.

If the team had limited time for every visit, they wouldn’t have had time to discuss everything with the patient. We all know that the visits to physicians are limited to 15-30 minutes. Without that limit, everyone could talk without clock ticking pressure. I learned a lot and hopefully contributed to knowledge exchange.
Moonika Raja completed her secondment at the Danish Nurses Organisation

My Secondment was in the Professional Department of Danish Nursing Organization (DNO) (Copenhagen, Denmark) with part of my time spent at the Danish Museum of Nursing History (DMNH) (Kolding, Denmark). DMNH shows the story of the history of nursing form the middle age to present. The museum was inaugurated in 1999 to celebrate the 100th anniversary of the DNO. The DMNH is housed in an authentic environment. The buildings were originally a tuberculosis sanatorium for children. In 1959, the sanatorium closed and from 1960 was Koldingfjord used by the National Department for the Care of the Mentally Deficient. In 1987, the Nurses’ Property Corporation bought the buildings. After an extensive renovations, Hotel Koldingfjord opened in 1990 and the museum in 1999. For nurses, the museum is a unique experience, and it is being used in the education for both nursing students and other healthcare students. You can read more about DMNH`s unique story by clicking here.
In the Danish Museum of Nursing History I was able to visit the historical exhibits charting historical and professional development of nursing in Denmark and was able to immerse myself and learn about the history of this important and significant place. I had possibility to work at the museum’s library but also with archival materials that were relevant to my research about older adult’s dignity in digitally-led healthcare. I mostly worked with documents about older adults’ care in Denmark and national digital strategies and innovative eHealth policies concerning older adults’ dignity in Scandinavian countries. I also learned about the museum’s research work.
In Copenhagen at my stay with Danish Nurses Organization’s Professional Department I learned about Professional Strategy 2023-2033: the aim of the new strategy and political themes covered in it. I learned more about nurses’ value to the society (nurses contribute with significant impact through their roles responding to the challenges of society and healthcare), their roles (nurses lead and develop the nursing profession), education (nurses’ education provides a solid professional foundation) and future good working life (nurses’ working lives should be in balance with everyday life and with room for professionalism). I learned about leadership skills and the DNO’s political work. It gave me a good example of how to involve team members in the working process. I was able to develop my coordinating skills and my skill to envision the future. The DNO currently represents 77,000 nurses. DNO’s vision is to stand stronger together for life as a nurse, save lives, prevent diseases, promote health, and strengthen the profession. This vision is based on values that include unity, empowerment and political and societal engagement .

I am very thankful to museum`s Director Trine Gjesing Antvor and Head of Professions in DNO Helle Winther Dahl for this wonderful opportunity to learn about their important work. I think this Secondment contributed to my research work and also helped me to develop different leadership skills.
Exchanging ideas and experiences: mobilizing knowledge
ESR Emma Jelstrup Balkin recently spent a few weeks visiting the Care Ethics department at the University of Humanistic Studies in Utrecht, Netherlands to share some of her findings and exchange ideas. This was a very rich experience, where Emma got to meet with many accomplished scholars and discuss ideas around existential meaning and well-being in ageing, care and nursing homes. She also got the chance to visit a Dutch nursing home, which was a wonderful opportunity to learn and gain new perspectives on how care is delivered in other countries. This nursing home, for example, has a focus on meaningful care. In this photo we are introduced to a 96-year-old resident who shared with us a little of her experiences with what it is like to live in a nursing home.

Read about our ESR Jayme Tauzer`s experience in her blog: Residential care in times of crisis: Preliminary experiences conducting ethnographic research in residential care during COVID-19. Read all here:


